Laura Keeler, R. Lee Kirby, Sherry Wang
Division of Kinesiology (Keeler), Division of Physical Medicine and Rehabilitation (Wang, Kirby), Dalhousie University, Halifax
ABSTRACT
Thirty-nine (39) wheelchair-using inpatients (17 females and 22 males ages 21-92 years), from the Nova Scotia Rehabilitation Centre completed a descriptive survey with the use of questionnaires to determine if two criteria were being met: 1) if inpatients have the wheelchair that they will be using or understand what arrangements are in place to obtain it prior to being discharged and 2) if they or their caregivers have received appropriate training in indoor and community wheelchair use or what arrangements are in place to receive such training after discharge. Twenty-three participants (59%) had the wheelchair they planned to use after discharge. Of the 16 who did not, 15 (94%) knew what arrangements were in place to obtain one. Twenty-two participants (56%) had received wheelchair skills training. Of the 17 who did not, none (0%) knew of arrangements to receive such training after discharge. Although almost all participants had their wheelchair or knew of arrangements to obtain one, a smaller portion received wheelchair skills training. These findings have implications for the wheelchair-provision process.
BACKGROUND
Wheelchair use is one of the most important tools for the mobility of people with impairments. Persons with limited mobility often require provision of a wheelchair; either manually propelled or powered depending on their functional level (WHO Guidelines, 2008). Evidence indicates that mobility devices improve activity, participation (Salminen, et al., 2009), and quality of life (Davies, De Souza, Frank, 2003). However, wheelchairs are not without problems, such as the frequent need for repairs (McClure, et al., 2009) and injuries (Gaal, et al., 1997). An important element of the wheelchair-provision process is wheelchair skills training.
Wheelchair Use at the Nova Scotia Rehabilitation Centre
For several years at the Nova Scotia Rehabilitation Centre (NSRC) site of the Capital District Health Authority (CDHA), the Wheelchair Skills Training Program (WSTP) has been used to train wheelchair users and/or their caregivers. Studies have shown that the WSTP is safe, effective and practical (MacPhee, et al., 2004; Best, et al., 2005; Kirby, et al., 2011; Ozturk et al,, 2011; Routhier et al., 2012). In its survey report of 2008, the Canadian Council on Health Services Accreditation identified the Wheelchair Skills Program (WSP) as one of two “leading practices”. The WSP has also been endorsed by management.
However, an inpatient stay at the NSRC is a busy period and many patients are reluctant to accept that a wheelchair will be needed for their future mobility needs. Also, the wheelchair-provision process is often incomplete at the time of discharge. For instance, a wheelchair prescription may have been deferred pending approval of a funding body or a prescribed wheelchair may not yet have been received. Anecdotally, we have observed that some patients are discharged without having received as much wheelchair skills training as might be appropriate.
PURPOSE
In the few days leading up to discharge, if a patient is to use a wheelchair thereafter, we believe that two criteria should be met:
- The wheelchair user should have the wheelchair that will be used or understand what arrangements are in place to obtain it.
- The wheelchair user and/or the caregiver should have received appropriate training in indoor and community wheelchair use or arrangements should be in place to receive such training after discharge.
The objective of this study was to determine if these two criteria are being met in our centre.
METHOD
Study Design
Descriptive survey study, with the use of questionnaires.
Participants
Thirty-nine participants were recruited. Each participant met the following inclusion criteria: was at least 18 years old, was medically stable, was willing to participate, was competent to provide informed consent, was able to communicate verbally, was an inpatient at the NSRC, had a length of stay of at least 2 weeks, was scheduled to be discharged from the NSRC within 72 hours of questionnaire administration, was currently using a wheelchair (power and/or manual) for at least 1 hour per day and was expected to be using a wheelchair after discharge. Potential participants were excluded if they failed to meet these criteria or if they had previously participated in a wheelchair-skills-training research study.
To describe the sample, demographic and clinical data were collected by interview and chart review.
Procedure
After recruitment, screening and informed consent, the contact information, demographic and clinical data were recorded from the participant and chart review. The questionnaire was administered and the wheelchair specifications were recorded.
Data Analysis
We entered the data into an Access database that was created for the purpose. Descriptive statistics were generated.
RESULTS
Table 1 describes the demographic and clinical data of participants collected during the study. Table 2 illustrates wheelchair provision information collected from interviewing participants. Table 3 illustrates wheelchair training information collected from interviewing patients.
|
Demographic and Clinical Data (N=39) |
|||
|
N | % | |
| Age (mean ± SD) |
|
57.3±19.0 | |
| Sex | |||
| Male | 22 | 56 | |
| Female | 17 | 44 | |
| Duration of Admission (mean ± SD days) | 66.8±51.6 | ||
| Discharge Destination | |||
| Home | 34 | 87 | |
| Long-term-care facility | 3 | 8 | |
| Other | 2 | 5 | |
| Diagnosis Accounting for Wheelchair Use | |||
| Limb amputation | 10 | 25 | |
| Multiple sclerosis | 7 | 18 | |
| Stroke | 4 | 10 | |
| Spinal cord injury | 6 | 15 | |
| Spinal bifida | 1 | 3 | |
| Other | 7 | 18 | |
| Myopathy | 2 | 5 | |
| Cerebral palsy | 1 | 3 | |
| Neuromuscular disease | 1 | 3 | |
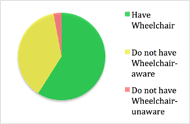 Figure 1: Participants who have and do not have their wheelchair they plan to use after discharge and which participants are aware of arrangements to obtain one
Figure 1: Participants who have and do not have their wheelchair they plan to use after discharge and which participants are aware of arrangements to obtain one Figure 1 illustrates the proportion of participants who had or did not have the wheelchair that will be used after discharge. It also shows the proportion of participants who did not have their wheelchairs but who did or did not understand what arrangements were in place to obtain the wheelchairs. Figure 2 illustrates the corresponding proportions for wheelchair skills training.
Wheelchair Provision (N=39) |
|||
|
N | % | |
|---|---|---|---|
Duration of Wheelchair use (mean ± SD years) |
4.5±7.6 | ||
| Daily Wheelchair use (mean ± SD hours) | 9.0±4.8 | ||
| Types of Wheelchairs Used | |||
| Manual | 23 | 59 | |
| Powered | 1 | 3 | |
| Both | 15 | 38 | |
| Owner of Wheelchair | |||
| Purchased | 14 | 36 | |
| Loaning | 20 | 51 | |
| Renting | 5 | 13 | |
Wheelchair Training (N=22) |
|||
|
N | % | |
Number of Training Sessions (mean ± SD) |
8.6±10.9 | ||
| Length of Training Sessions (mean ± SD min) | 37.9± 19.2 | ||
| Enjoy Wheelchair Training? | |||
| Yes | 18 | 82 | |
| No | 4 | 18 | |
| Recommend to others? | |||
| Yes | 22 | 100 | |
| No | 0 | -- | |
After the 39 participants were interviewed 1-3 days prior to their anticipated discharge dates, over half had the wheelchairs they planned to use after being discharged and had received wheelchair skills training. Fifty-nine percent (59%) of participants (N=23) had the wheelchairs that they planned to use, whereas 41% (N=16) did not. Of those participants who did not have the wheelchair they planned to use, 94% (N=15) understood what arrangements were in place to obtain it.
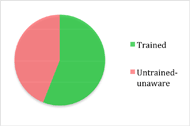 Figure 2: Participants who have and have not received wheelchair skills training and which participants are aware of arrangements to receive training after discharge
Figure 2: Participants who have and have not received wheelchair skills training and which participants are aware of arrangements to receive training after discharge Fifty-six percent (56%) of participants (N=22) received wheelchair skills training, whereas 44% (N=17) did not. Of those participants who did not receive training, none were aware of any arrangements that had been made to receive training after discharge.
The average number of training sessions reported was 8.6, ranging from 1-45 sessions, lasting an average of 37.9 minutes. Eighty-one percent (81%) of participants (N=18) enjoyed the wheelchair skills training, and all would recommend the training to others.
A number of participants provided verbal feedback on the process of being trained to use a wheelchair. When participants were asked why they had not received wheelchair skills training during the current admission, the majority answered with “already knew how to use a wheelchair” or “did not need any training”. The feedback regarding wheelchair skills training was very positive, with most participants stating they learned a lot.
DISCUSSION
The Wheelchair Skills Training Program (WSTP) has been used to train wheelchair users and/or their caregivers at the NSRC. However, we have observed that some patients are discharged without having received an appropriate amount of wheelchair skills training. Also, at the time of discharge, the wheelchair provision process may be incomplete for some patients.
The current study found almost all participants had the wheelchair they planned to use after discharge or knew what arrangements were in place to obtain them. A smaller portion had received wheelchair skill training, and those who did enjoyed the training. The number of training sessions varied extensively, which may reflect the different individual needs of participants. It may also reflect how participants could have misinterpreted “wheelchair training skills” for another aspect of therapy. Of those who reported that they had not received training, none were aware of any future plans to obtain it.
Study limitations include the small sample size and heterogeneous nature of the participant sample. Future study will be needed to address these limitations, to look into factors (e.g. diagnosis) that might affect the prevalence of training and better explore the reasons why the prevalence of training was suboptimal.
CONCLUSION
Although most wheelchair users at the time of discharge from the NSRC had received their wheelchairs or understood the arrangement in place, almost half reported that they had not received any training during their current admission in how to use their wheelchairs and were unaware of any plans to receive it.
REFERENCES
Best, K.L., Kirby, R.L., Smith, C., & MacLeod, D.A. (2005) Wheelchair skills training for community-based manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil. Dec, 86(12), 2316-23.
Davies, A., De Souza, L.H., & Frank, A.O. (2003). Changes in the quality of life in severely disabled people following provision of powered indoor/outdoor chairs. Disabil Rehabil , 25, 286-90.
Gaal, R.P., Rebholtz, N., Hotchkiss, R.D., & Pfaelzer, P.F. (1997). Wheelchair rider injuries: causes and consequences for wheelchair design and selection. J Rehabil Res Dev, 34, 58-71.
Kirby, R.L., Mifflen, N.J., Thibault, D.L., Smith, C., Best, K.L., Thompson, K.J., & MacLeod, D.A. (2004). The manual wheelchair-handling skills of caregivers and the effect of training. Arch Phys Med Rehabil, 85(12), 2011-9.
MacPhee, A.H., Kirby, R.L., Coolen, A.L., Smith, C., MacLeod, D.A., & Dupuis, D.J. (2004). Wheelchair skills training program: A randomized clinical trial of wheelchair users undergoing initial rehabilitation. Arch Phys Med Rehabil, 85(1), 41-50.
McClure, L.A., Boninger, M.L., Oyster, M.L., Williams, S., Houlihan, B., Lieberman, J.A., & Cooper, R.A. (2009). Wheelchair repairs, breakdown, and adverse consequences for people with traumatic spinal cord injury. Arch Phys Med Rehabil, 90, 2034-8.
Ozturk, A., & Ucsular, F.D. (2011). Effectiveness of a wheelchair skills training programme for community-living users of manual wheelchairs in Turkey: a randomized controlled trial. Clin Rehabil, 25, 416-24.
Routhier, F., Kirby, R.L., Demers, L., Depa, M., & Thompson, K. (2012). Efficacy and retention of the French-Canadian version of the Wheelchair Skills Training Program for manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil, 93, 940-8.
Salminen, A.L, Brandt, A., Samuelsson, K., Toytari, O., & Malmivaara, A. (2009). Mobility devices to promote activity and participation: A systemic review. J Rehabil Med, 41(9), 697-706.
World Health Organization. (2008). Guidelines on the provision of manual wheelchairs in less-resourced settings.